It is generally said that coma is the most severe form of altered consciousness. But what is consciousness? Philosophers, psychologists, physiologists, neurobiologists … everyone has a definition. We will approve that from the doctor. For him, it is a state of physiological cerebral activation (wakefulness), which allows him to perceive the outside world, and to adapt his responses (primary or complex) to requests. Specifically, the comatose patient does not react or react inappropriately to stimuli from the outside world.
In practice, for neurosurgeons and resuscitators, a coma occurs suddenly after a head injury, stroke, sudden drop in the oxygen supply, or even meningoencephalitis. Immediately, two questions appear, raw and direct. How severe is coma, meaning its depth? What is the likelihood that the patient will return to normal consciousness?
Four phases, three developments?
To answer these questions, we have long relied on classifying four stages of coma. To know:
-
Stage 1, when contact is reduced but possible;
-
The second stage, when there is no communication but reactions to painful stimuli;
-
Stage 3, when the patient does not react at all to painful stimuli;
-
Stage 4, when life is only preserved by artificial means: This is called a passed coma.
In addition, three changes were visualized: improvement with improved cognition and reaction, brain death followed by patient death, or a vegetative coma.
This vegetative state It was defined in 1994 As “a clinical state devoid of any (manifestation of) awareness of self and the environment, associated with the existence of the wakefulness / sleep cycle with the complete or partial maintenance of the automatic functions of the hypothalamus and the brainstem.” A condition in which the eyes are open, and reflexive movements are present, but where there is no reaction to verbal commands or other stimulation – leading some to view it as Functional awakening without a conscious mental life and without awareness of the surrounding world.
However, advances in resuscitation in recent decades have helped to keep patients with significant brain damage alive. Meanwhile, there are new pathways for physiological exploration, such as Positron emission tomography (PET) and above all Professional in magnetic pictograms (IRMf) It overturns perceptions of perception and interaction in the comatose patient, and thus the boundaries of disturbances of consciousness.
Lateral disturbances on two scales
To assess the depth of coma, its four stages in use since World War II show its limits. A tool was necessary that remained easy to use, giving identical results from one examiner to another, but its evaluation was more accurate. And then the use of the Glasgow Scale or GCS scale was developed, Originally designed To assess the severity of coma in adults after head trauma.
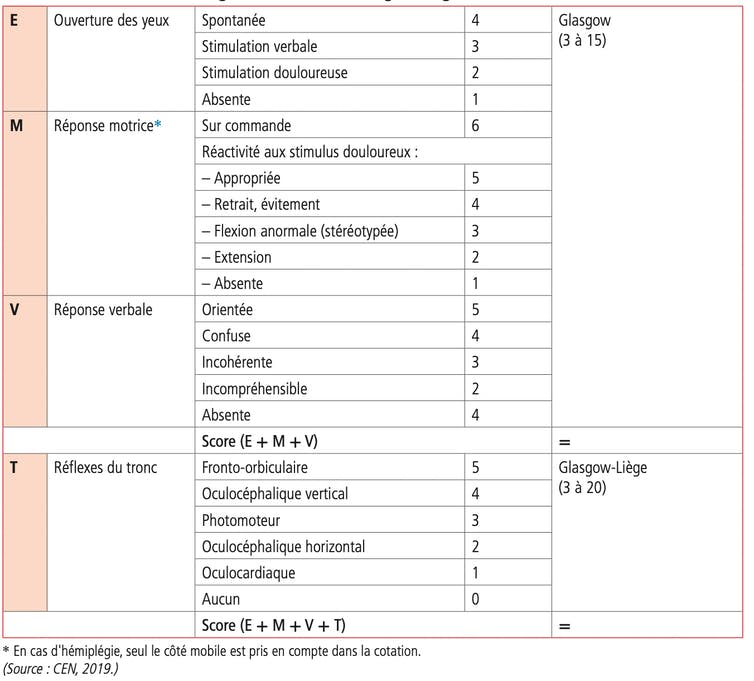
Its use soon extended to other groups of patients, sometimes with variations (for example in pediatrics, or for deep coma), and GCS became the most widely used finding in the world. Three criteria are evaluated: eye opening, coded in 4, verbal response, marked at 5, and motor response, marked at 6. Total scores range from 3 (deep coma) to 15 (consciousness. Normal). And we talk about coma or loss of consciousness when the patient has a score of less than 8.

Despite its simplicity, the Glasgow scale does not always give the same results depending on who uses it. In addition, it suffers from several usage restrictions. For example, for verbal evaluation of patients with speech impairment or intubation. Or for visual evaluation in the case of orbital edema. But also, when it comes to choosing which side to keep in case the motor response is asymmetric. Finally, it does not make it possible to differentiate coma from Bulging syndrome (closure syndrome)The subject is completely paralyzed, but nonetheless conscious.
To remedy these problems, in 1982, Jacques Bourne’s Belgian team added to the Glasgow scale assessing several brainstem reflexes, which were rated from 5 to 0: orbital anterior reflexes, vertical vertical reflexes, and optical reflexes. So he called Glasgow Liege (GLS), and with scores ranging from 3 to 20, this scale allows for a more detailed assessment of the severity of deep coma, at the lowest score (3 or 4).
However, a problem remained: the GLS score did not appear to be more sensitive than the GCS score in assessing residual consciousness during the vegetative state. Indeed, patients for whom such a diagnosis was made were presented Temporary signs of consciousness, With continued gaze, tears or smiles, and even gestures, in response to a strong emotional stimulus (their reflection in the mirror, the presence of loved ones, music associated with a vivid memory …).
It was to take into account these transient signs, but above all the very fluctuating signs of consciousness that are understandable Minimum awareness Or altered, which we also call the anemia. Four years later, in Cambridge, neuroscientist Adrian Owen and his team published a book Work is as innovative as it is subversive. Based on functional magnetic resonance imaging (fMRI), this study showed a conserved consciousness in a young patient diagnosed with a vegetative state: When asked to “imagine playing tennis or moving around your home, the same cortical areas were activated as in healthy volunteers.”
Use of imaging methods
Therefore, the use of different strategies to explore the metabolism (positron emission tomography and functional magnetic resonance imaging) or electrical activity (EEG) of the brain has evolved. The examination consists of measuring brain activity at rest, when the patient is asked to perform cognitive tasks, or when exposed to external stimulation. More than once in ten, we find that despite his “vegetative state,” the patient is able to follow the instructions.
So these functional pictorial methods reveal that the “vegetative state” is far from matching what its name means – not to mention the connotation of disdain. Even so in 2010, the Belgian national team, Stephen Lloris He suggested replacing it with another: “unresponsive arousal syndrome”.
Ultimately, today, the level of change in patients’ consciousness is no longer determined solely by their visual, verbal, kinesthetic, or reflexive reactions to stimuli, but also by more detailed measurements of the brain’s metabolic activity. One can imagine the new investigation methods such as Electrical stimulation And the Virtual Reality Tomorrow we will define it differently: Our team will soon launch a clinical trial based on virtual reality to wake up from a coma.
Likewise, we can hope that future brain and machine interfaces will provide all of these patients the possibility to interact with stimuli from the outside world, or even communicate. Undoubtedly, such a development would not fail to open a complex ethical debate.
In France, there are currently about 1,500 patients in an unresponsive state of wakefulness or altered consciousness.

“Certified gamer. Problem solver. Internet enthusiast. Twitter scholar. Infuriatingly humble alcohol geek. Tv guru.”





